
As the COVID-19 pandemic continues to spur unprecedented growth for telehealth and remote patient monitoring technology, it’s clear that a home-based model of care is here to stay. Front and center to these changes are remote patient monitoring (RPM) programs, which allow patients to collect their own biometric data from home, communicate virtually with clinicians, and play a more active role in their treatment plan. Below are three ways that payers can leverage RPM solutions in order to improve member satisfaction.
Self-management
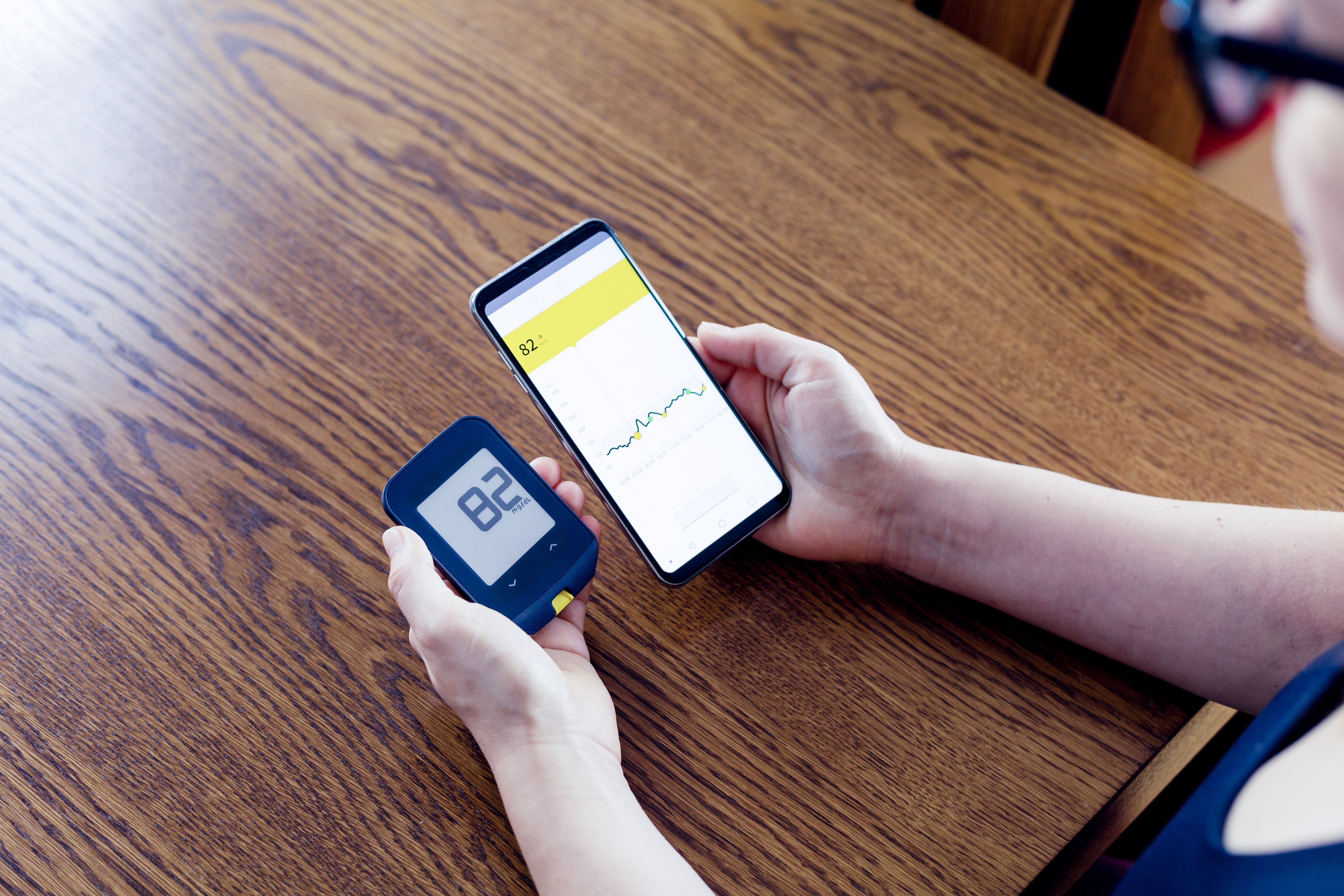
Remote patient monitoring tools empower patients to take a more active role in their care plan. With over 81% OF ALL AMERICANS having a smartphone, patients can monitor their biometrics, view educational content, communicate with care teams, and access more resources from the palm of their hand.
This self-management can lead to significant cost reductions as well. Chronic care management accounts for over 85% of all healthcare spending, and many modern RPM and telehealth solutions allow patients to manage portions of their chronic condition from home. With a healthcare-at-home model of chronic care, patients are more likely to be proactive in their care and avoid expensive hospital stays. In a 2018 RPM SURVEY sponsored by Healthcare Dive, 38% of healthcare organizations stated that remote patient monitoring resulted in fewer patient admissions.
Personalized Care
With telehealth and RPM solutions, payers can tailor a treatment plan specifically to each patient’s needs. Providers can offer personalized incentives, education opportunities, and treatment experience based on each individual’s interests and accessibility level. Additionally, RPM triggers can be based on each patient’s specific condition, risk profile, and biometric data, rather than a “cookie cutter” approach to care. This allows patients to receive treatment in their preferred way, rather than a one-size-fits-all approach to treatment.
We recently spoke with Kent Dicks, CEO of Life 365, a leading telehealth and remote care management provider, on how this personalization can create better patient engagement.:
“Our models of data-driven care need to take into account who you are as an individual and personalize care to you, which is where empathy comes in. We can’t approach every patient with the same model and the same need because everyone has different requirements.
I would always joke with my mom that if she would just take her regular blood pressure readings and medication on a daily basis, then we would send her a Netflix gift card. People would say ‘Oh gosh, she needs to be out exercising instead. You should send her a silver sneakers membership”. But y’know? That wouldn’t have worked for her, my mom walked around 300 steps a day. A silver sneakers membership would not have properly incentivized and engaged her in her care. It’s not personalized.”
To listen to our full interview with Kent, LISTEN & SUBSCRIBE ON APPLE PODCASTS.
Improved Star Ratings
Lastly, remote patient monitoring improves payer’s star rating, CMS’s quality rating metric. With over 78% of all Medicare beneficiaries choosing to enroll in programs with high (4+) star ratings, RPM programs are a practical way for payers to expand their membership. Payers who provide remote patient monitoring boast higher treatment adherence and better patient outcomes, with over 13% of survey respondents remarking that RPM “improves patient compliance”.
VectorCare is proud to announce that WE’VE RECENTLY PARTNERED WITH LIFE 365 TO OFFER REMOTE PATIENT MONITORING SERVICEs. Payers can now use the VectorCare platform to order remote care kit delivery in minutes, making it simpler than ever to set up remote monitoring solutions upon patient discharge. Click here to learn more.
Want to read more from the Patient Care Logistics Journal? Check out our latest podcast episode with Kent Dicks, the CEO and founder of Life365.
Similar resources

How Lyft as a SMART on FHIR App Enables Faster Discharges and Reduces Readmissions



